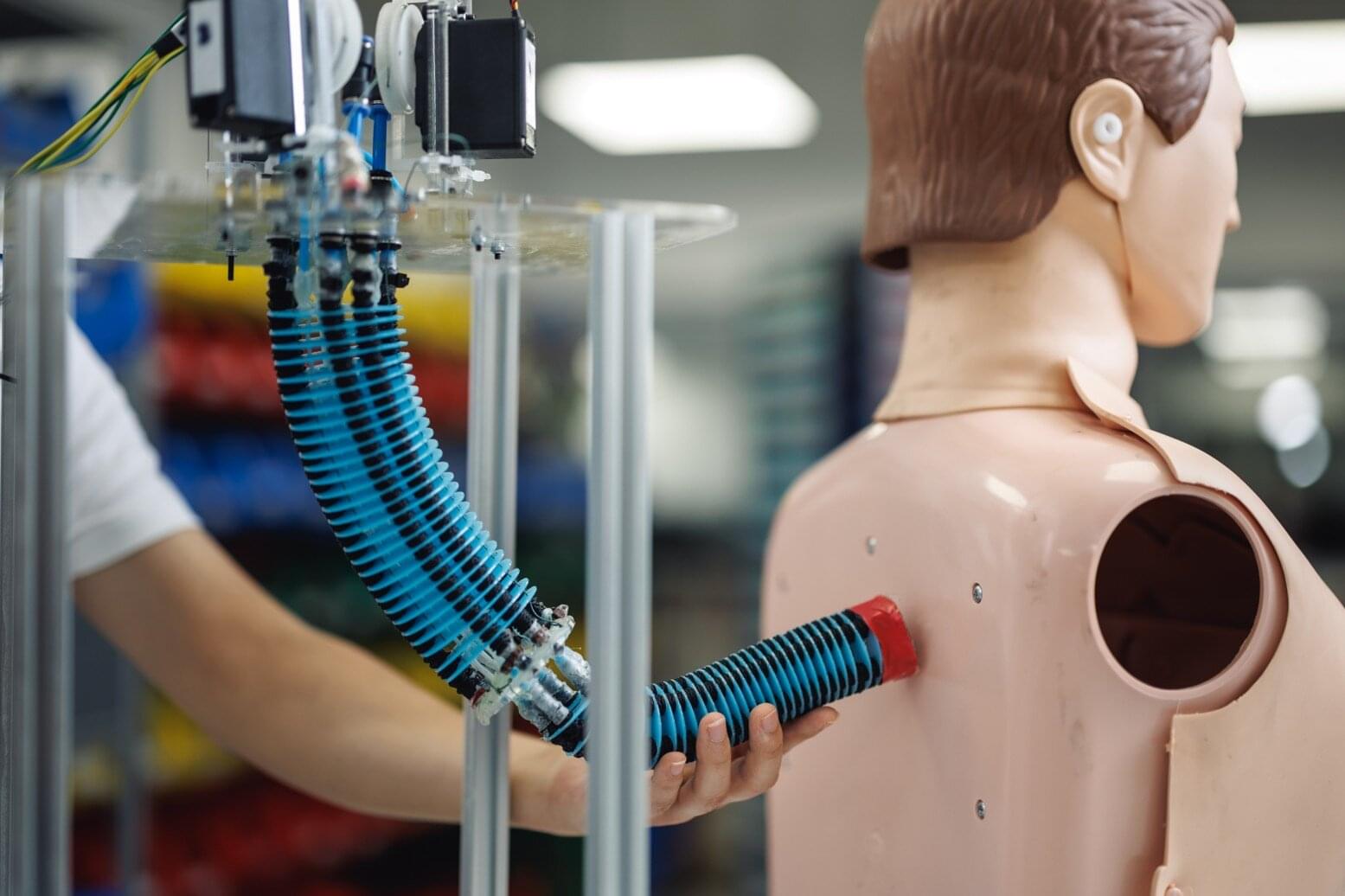
The human body continuously generates a rich spectrum of vibrations—often without us ever noticing. Everyday unconscious activities such as breathing, speaking, and swallowing all produce subtle yet distinct mechanical signals. Although these faint vibrations carry valuable information about physiological state, they have long been difficult to capture accurately using conventional wearable devices.
Recently, a research team led by Professor Kilwon Cho of the Department of Chemical Engineering at Pohang University of Science and Technology (POSTECH), along with Ph.D. candidate Kang Hyuk Cho and postdoctoral researcher Dr. Jeng-Hun Lee, has developed a wearable vibration sensor capable of precisely detecting these subtle yet highly dynamic signals, without requiring any external power source. This breakthrough opens new possibilities for wearable medical and health care technologies and demonstrates strong potential as a core sensing platform for next-generation smart devices. The work was published in the inaugural issue of Nature Sensors.
Sounds produced by the human body span a wide range of frequencies. Physiological signals such as breathing, swallowing, and speech typically occur at lower frequencies, while sounds such as coughing or groaning emerge at relatively higher frequencies. Accurately capturing these signals requires precise detection of the minute vibrations transmitted to the skin surface across a broad frequency spectrum.