Schmauck-Medina et al. review dietary restriction as a class of geroprotective interventions, considering evidence across species, conflicting data, mechanisms, side effects and pharmacological mimetics.


Scientists are discovering that targeting senescent cells the “aged” cells surrounding tumors may weaken cancer itself.
Cancer often forces nearby cells into accelerated aging. Those senescent cells then release growth factors that help the tumor survive and expand.
A new therapy called Senovax aims to eliminate those surrounding cells, effectively collapsing the tumor’s support system.
Preclinical data from Immortebio shows tumor reduction in mouse models of:
Lung cancer.


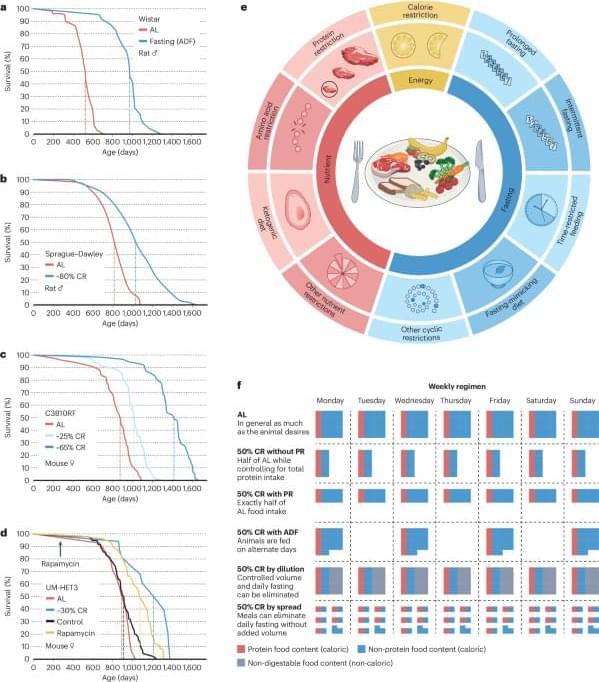
Defined as reduced caloric intake or selective limitation of specific nutrients without malnutrition, is one of the most robust interventions known to extend lifespan and healthspan across species. Studies from yeast to mammals demonstrate that DR elicits conserved genetic, transcriptional, and epigenetic programs that promote cellular maintenance and stress resistance. At the molecular level, DR engages evolutionarily conserved nutrient-sensing pathways, including insulin/IGF-1 signaling (IIS), the mechanistic target of rapamycin (mTOR), AMP-activated protein kinase (AMPK), and NAD+-dependent sirtuins, which converge on key transcription factors (TFs) and transcriptional coactivators (TCs) to coordinate metabolic and longevity-associated gene expression. Downstream, these pathways enhance autophagy and proteostasis, remodel mitochondrial function and redox balance, reshape immune and inflammatory networks, and induce epigenetic and transcriptional reprogramming. Recent work further highlights amino acid–specific sensing mechanisms, endocrine mediators such as fibroblast growth factor 21 (FGF21), the gut microbiome, circadian regulators, and nuclear pore–associated transcriptional plasticity as integral components of DR responses. Importantly, the physiological outcomes of DR are context dependent and influenced by genetic background, sex, age at intervention, and the type and duration of restriction. In this review, we summarize current knowledge on the genetic and molecular architecture underlying DR-induced longevity and health benefits across species, discuss implications for aging-related diseases, and outline future directions toward precision nutrition and safe translational strategies.
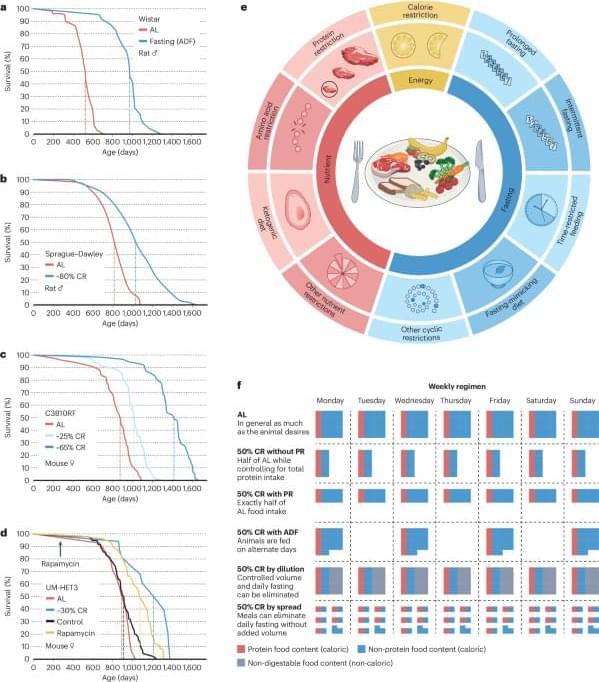
Aging is characterized by a progressive decline in physiological integrity, reduced stress resilience, and increased susceptibility to chronic diseases (Lopez-Otin et al., 2023). Among numerous genetic, pharmacological, and lifestyle interventions examined over the past decades, dietary restriction (DR) remains the most robust and evolutionarily conserved strategy for extending lifespan and improving healthspan. Originally described in rodents nearly a century ago, the beneficial effects of reduced nutrient intake have since been validated in a wide range of organisms, including yeast, nematodes, flies, and mammals (Wu et al., 2022). While often used interchangeably, it is critical to distinguish between different nutritional interventions to avoid conceptual overlap. Caloric restriction (CR) typically refers to a chronic reduction in total calorie intake (usually 20%–40%) without malnutrition.

Exposure to indoor air pollution during childhood tends to be linked to poorer cognitive health in older adulthood. This suggests that access to clean energy early in life might help protect the brain as it ages. These findings come from a recent study published in Social Science & Medicine, which provides evidence that growing up in homes using solid fuels for cooking can set off a chain of disadvantages that affect memory and thinking skills decades later.
Xu Zong conducted the new study to explore a gap in our understanding of how early environmental exposures shape aging. While many scientists have established that breathing polluted air during adulthood increases the risk of cognitive decline, the long-term impact of breathing indoor air pollution during childhood remained mostly unexplored. Around the world, billions of people still rely on solid fuels like coal and wood for daily cooking and heating. This practice fills homes with toxic pollutants.
“I am interested in understanding how early-life living conditions, specifically indoor air pollution, may have long-term consequences for cognitive health. Air pollution has been highlighted by The Lancet as one of the modifiable risk factors for dementia. While much research has focused on adult exposures or urban outdoor pollution, there was a gap in linking childhood indoor environments to cognitive outcomes later in life,” said Zong, a researcher at the Max Planck – University of Helsinki Center for Social Inequalities in Population Health.

“Glass” has a unique and distinct meaning in physics—one that refers not just to the transparent material we associate with window glass. Instead, it refers to any system that looks solid but is not in true equilibrium and continues to change extremely slowly over time. Examples include window glass, plastics, metallic glasses, spin glasses (i.e., magnetic systems), and even some biological and computational systems.
When a liquid is cooled very quickly—a process called quenching—it doesn’t have time to organize into a crystal but becomes stuck in a disordered state far from equilibrium. Its properties—like stiffness and structure—slowly evolve through a process called “aging.”
Now, a research team from the Institute of Theoretical Physics of the Chinese Academy of Sciences has proposed a new theoretical framework for understanding the universal aging behavior of glassy materials. The study is published in the journal Science Advances.

Researchers have identified a new type of blood-based biomarker test for Alzheimer’s disease that measures structural changes in proteins, providing more information on the underlying biology of the disease than standard blood tests. The findings, published in Nature Aging, also provide new insights into how Alzheimer’s disease biology may differ between males and females.
“This work introduces a fundamentally new, blood-based approach to detecting and staging Alzheimer’s disease,” said Dr. Richard Hodes, director of NIH’s National Institute on Aging (NIA). “By revealing protein structural changes associated with genetic risk, symptom severity, and sex differences—features not captured by existing biomarkers—this research could enable earlier diagnosis and more effective clinical trials.”