Johns Hopkins University researchers have grown a novel whole-brain organoid, complete with neural tissues and rudimentary blood vessels—an advance that could usher in a new era of research into neuropsychiatric disorders such as autism.
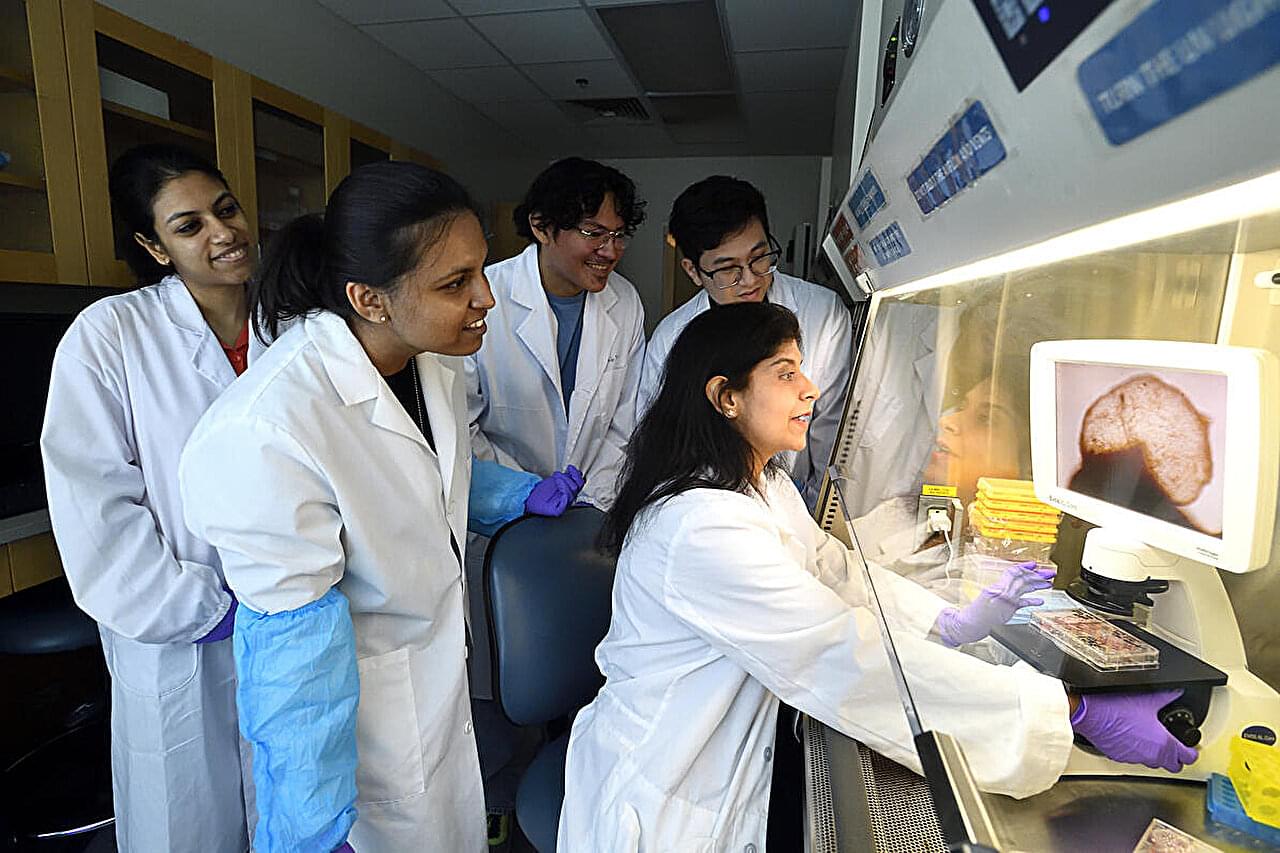
“We’ve made the next generation of brain organoids,” said senior author Annie Kathuria, an assistant professor in JHU’s Department of Biomedical Engineering who studies brain development and neuropsychiatric disorders. “Most brain organoids that you see in papers are one brain region, like the cortex or the hindbrain or midbrain. We’ve grown a rudimentary whole-brain organoid; we call it the multi-region brain organoid (MRBO).”
The research, published in Advanced Science, marks one of the first times scientists have been able to generate an organoid with tissues from each region of the brain connected and acting in concert. Having a human cell-based model of the brain will open possibilities for studying schizophrenia, autism, and other neurological diseases that affect the whole brain—work that typically is conducted in animal models.