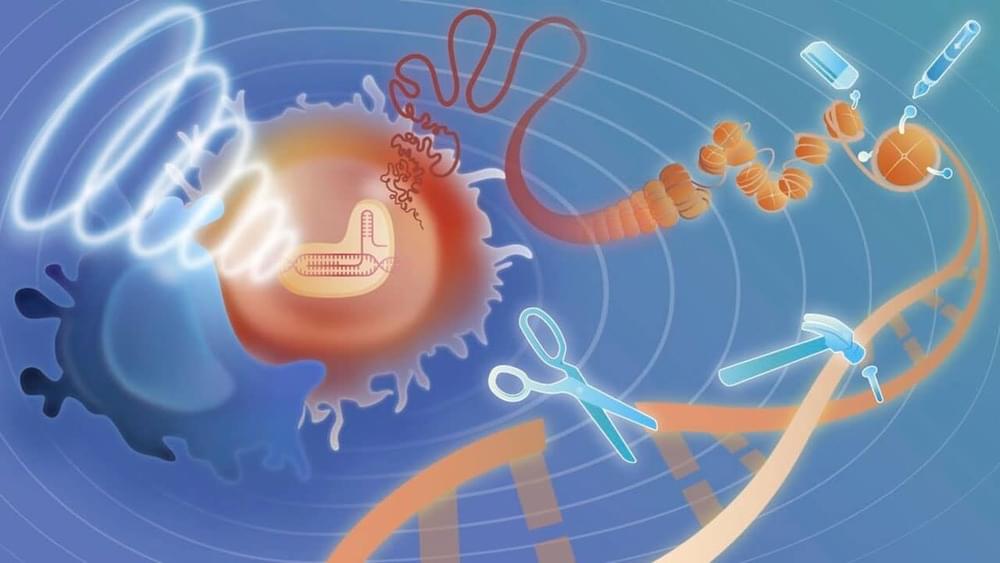
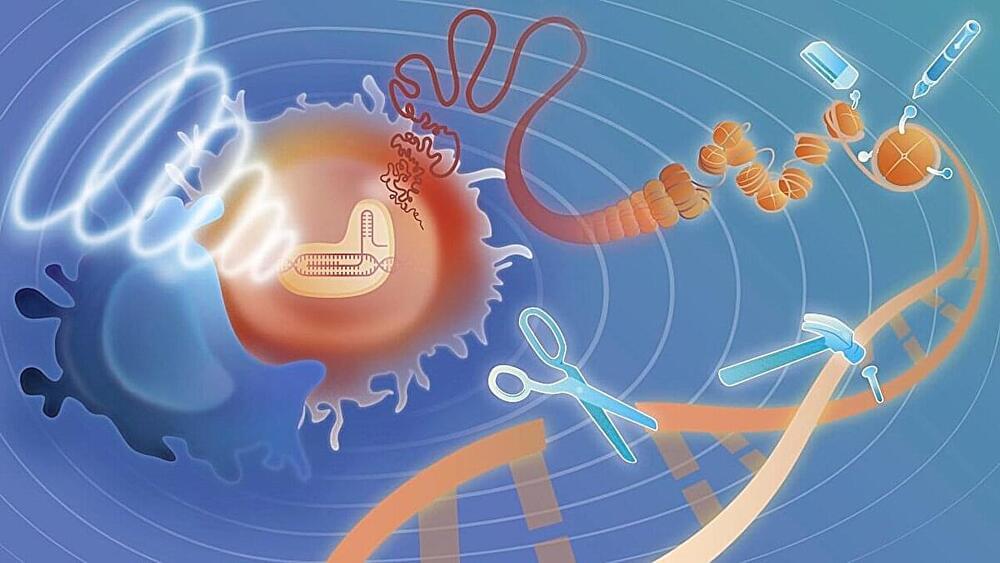
Summary: Researchers identified a brain circuit involving the amygdala and hippocampus that predicts resilience to stress in mice. Mice with disrupted neural communication in this circuit struggled to seek rewards, but activating the neurons restored resilience and improved decision-making.
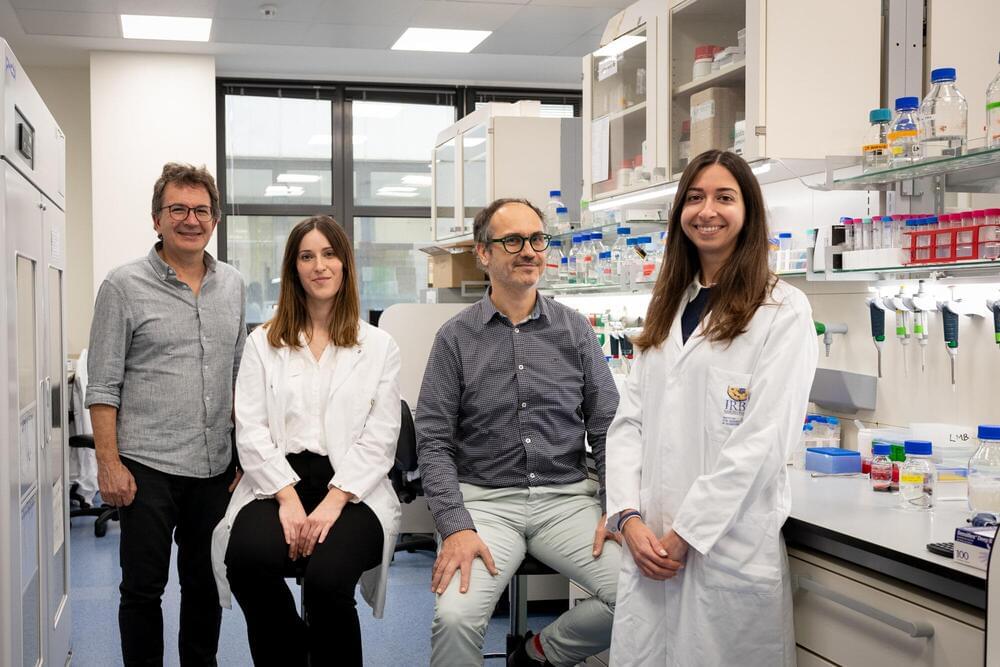
Using chemogenetics, the team stimulated brain activity in less resilient mice, which then displayed normal behavior and sought sweetened water. This breakthrough suggests potential new, non-invasive treatments for chronic stress and depression in humans, with researchers now exploring similar patterns in human brains.