Organoids are an improved model for the study human biology and disease, because they are miniaturized versions of human organs and tissues. | Cell And Molecular Biology.
Category: biotech/medical – Page 822
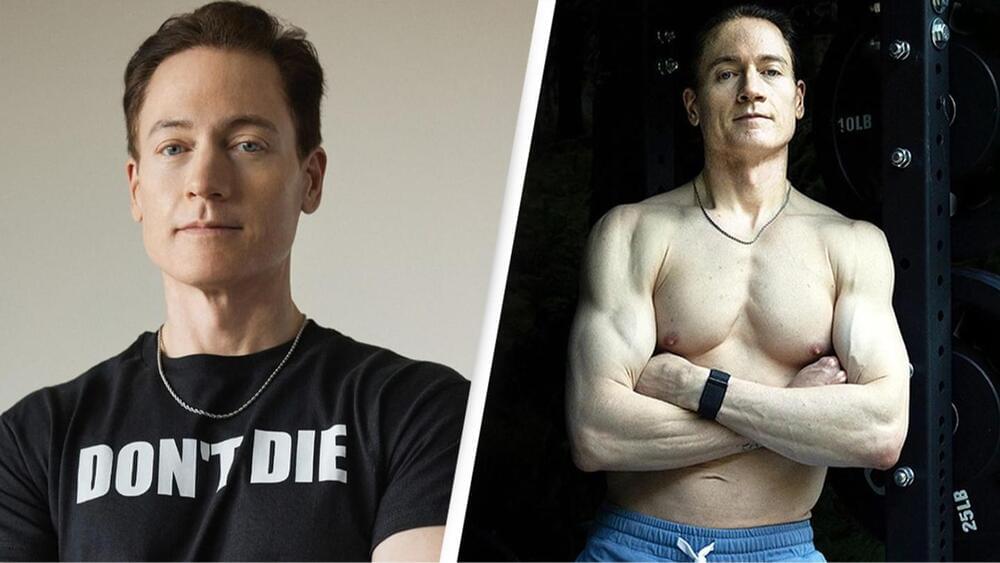
Biohacker who is ‘reverse aging’ reveals $20k medical procedure that ‘edits his DNA’ so he ‘lives forever’
He added: “Their target: follistatin gene therapy. A pioneering technology with the potential to improve muscle and strength [and] slow the speed of aging and many more benefits.”
The millionaire explained that the procedure involves an injection in the stomach and in the buttocks.
It also costs $20,000, so not exactly cheap.
Scientists pioneer new ultrasound technology that can scan the brain
Scientists have achieved groundbreaking brain mapping using ultrasound, detailed in a May 2024 Science Translational Medicine paper. Led by Richard Andersen and Charles Liu, they developed a non-invasive method to monitor brain activity with unprecedented clarity. This innovation, employing an ‘acoustically transparent’ skull window, allows real-time observation of neuronal and blood flow dynamics. The technique promises new insights into brain function and potential advancements in treating neurological disorders, marking a transformative milestone in neuroscience.

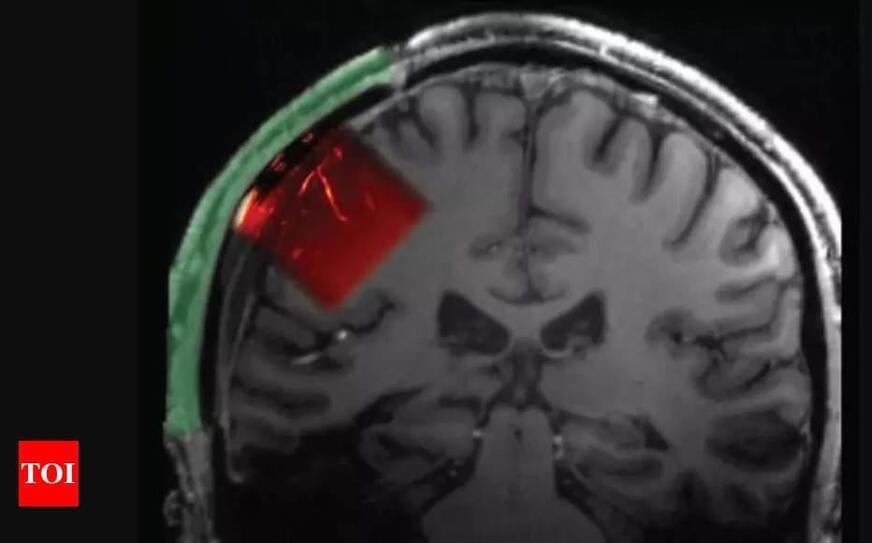
Study Suggests Computerized Brain Implant Could One Day Decode Internal Speech for Those Who Can No Longer Speak
The ability to communicate using only your thoughts might sound like the stuff of science fiction. But for people who don’t have the ability to speak or move due to injury or disease, there’s great hope that this may one day be possible using brain-computer interfaces (BCIs) that can “read” relevant brain signals and translate them into written or spoken words. A research team has made a preliminary advance in this direction by showing for the first time that a computerized brain implant can decode internal speech with minimal training.
In the new NIH-supported study, researchers implanted such a device in a brain area known to be important for representing spoken words called the supramarginal gyrus in two people with tetraplegia, a condition marked by full body paralysis from the neck down due to cervical spinal cord injury. The researchers found that the device could decode several words the participants “spoke” only in their minds. While we are far from using such a device to decode whole sentences or even phrases, and the exact mechanisms of internal speech are still under study, the findings, reported in Nature Human Behavior, are notable because it had been unclear whether the brain signals involved in thinking words could be reproducibly translated.
The findings come from a team led by Richard Andersen at the California Institute of Technology, Pasadena, CA, and Sarah Wandelt, now at the Feinstein Institutes for Medical Research in Manhasset, NY, and the study was supported by the NIH Brain Research Through Advancing Innovative Neurotechnologies® (BRAIN) Initiative Research Opportunities in Humans program. Though earlier research had shown that brain implants could decode vocalized, attempted, and mimed speech, it had yet to be seen whether internal speech could be similarly decoded.
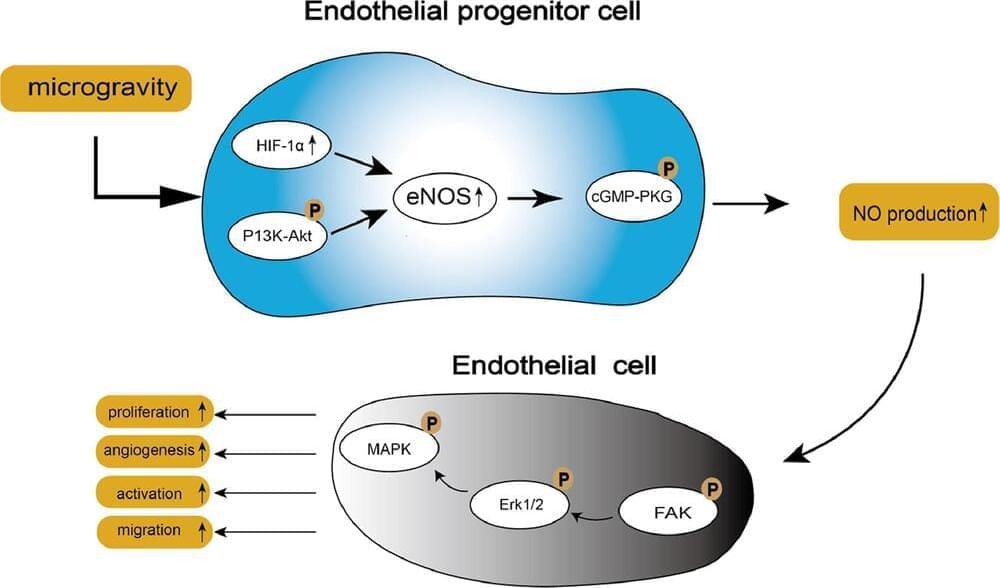
Cells grown in microgravity show 3D structures that could be used in medicine
Humanity is on the verge of entering a new era of space exploration, with the Artemis III mission planning to return humans to the moon in 2026, for the first time in 50 years. Not only will Artemis see a woman and a person of color walk on the lunar surface for the first time, but the week-long mission to the south pole of the moon will begin a period of longer and longer stays in space.

Decoding Heart Rate Signals To Refine Brain Stimulation Therapies for Depression
Study suggests heart rate may be a useful tool to determine where to stimulate the brains of individuals with depressive disorders when brain scans aren’t available.
New research suggests a common brain network exists between heart rate deceleration and depression. By evaluating data from 14 people with no depression symptoms, the team of researchers at Brigham and Women’s Hospital, a founding member of the Mass General Brigham healthcare system, found stimulating some parts of the brain linked to depression with transcranial magnetic stimulation (TMS), also affected heart rate, suggesting clinicians may be able to target those areas without the use of brain scans that aren’t widely available. The findings were published recently in the journal Nature Mental Health.
Heart-Brain Coupling and TMS.
Dutch develop no-pain needle-free injections
Researchers in the Netherlands are developing ‘virtually painless’ injections without needles in what they hope is a breakthrough that will ease fear and encourage vaccinations.
#News #Reuters #BubbleGun #NeedleFree #Vaccine.
Subscribe: http://smarturl.it/reuterssubscribe.
Reuters brings you the latest business, finance and breaking news video from around the globe. Our reputation for accuracy and impartiality is unparalleled.
Get the latest news on: http://reuters.com/
Follow Reuters on Facebook: / reuters.
Follow Reuters on Twitter: / reuters.
Follow Reuters on Instagram: https://www.instagram.com/reuters/?hl=en
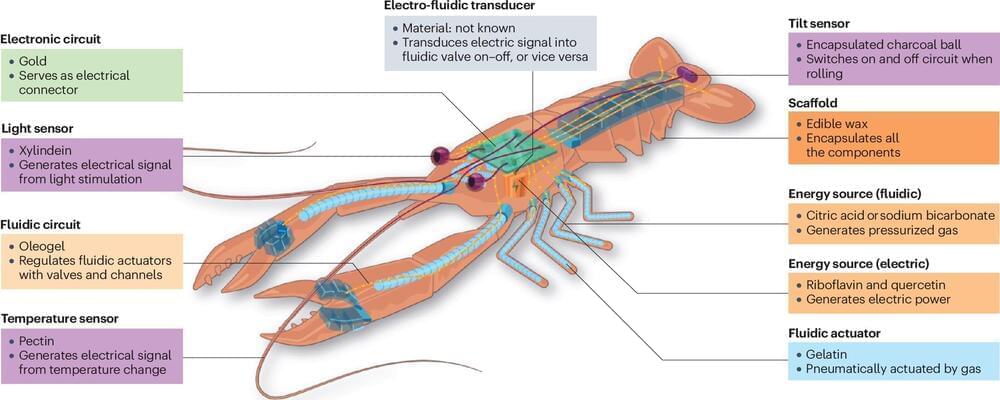
A fully edible robot could soon end up on our plate, say scientists
Science and Technology: Some robots could be “eaten” so they could walk around inside the body and perform tests or surgeries from the inside out; or administer medications.
Robots made of several nanorobots joined together could assemble and reassemble themselves inside the body even after being…
Robots and food have long been distant worlds: Robots are inorganic, bulky, and non-disposable; food is organic, soft, and biodegradable. Yet, research that develops edible robots has progressed recently and promises positive impacts: Robotic food could reduce electronic waste, help deliver nutrition and medicines to people and animals in need, monitor health, and even pave the way to novel gastronomical experiences.
But how far are we from having a fully edible robot for lunch or dessert? And what are the challenges? Scientists from the RoboFood project, based at EPFL, address these and other questions in a perspective article in the journal Nature Reviews Materials.
“Bringing robots and food together is a fascinating challenge,” says Dario Floreano, director of the Laboratory of Intelligent Systems at EPFL and first author of the article. In 2021, Floreano joined forces with Remko Boom from Wageningen University, The Netherlands, Jonathan Rossiter from the University of Bristol, UK, and Mario Caironi from the Italian Institute of Technology, to launch the project RoboFood.
Melanoma Skin Cancer Development Time Lapse (Normal to Stage 4 Melanoma Over 10 Years)
Using generative AI, this time lapse sequence shows how melanoma skin cancer develops over 10 years. Starting with normal skin, slow progression to stage 4 melanoma is shown.
Obviously, such a time lapse can not be realistically accomplished as there is no way to know if any given area of skin will turn into cancer. Obviously, somebody with such future knowledge would have to start taking such photos now in the same spot over next 10 years to watch it slowly turn into cancer.
Watch time lapse video of basal cell carcinoma: https://youtube.com/shorts/d_O5zHgKnP8
Watch this video to see how these can be surgical removed: https://youtu.be/Op3zYytUDDs.
Video created by Dr. Christopher Chang: