Microwave technology has dramatically progressed, marked by the arrival of the 5G era, owing to the advantages of electromagnetic waves in long-distance, wireless, and high-speed transmissions. However, electromagnetic wave pollution problems such as electromagnetic wave interference and electromagnetic wave radiation are becoming increasingly serious.
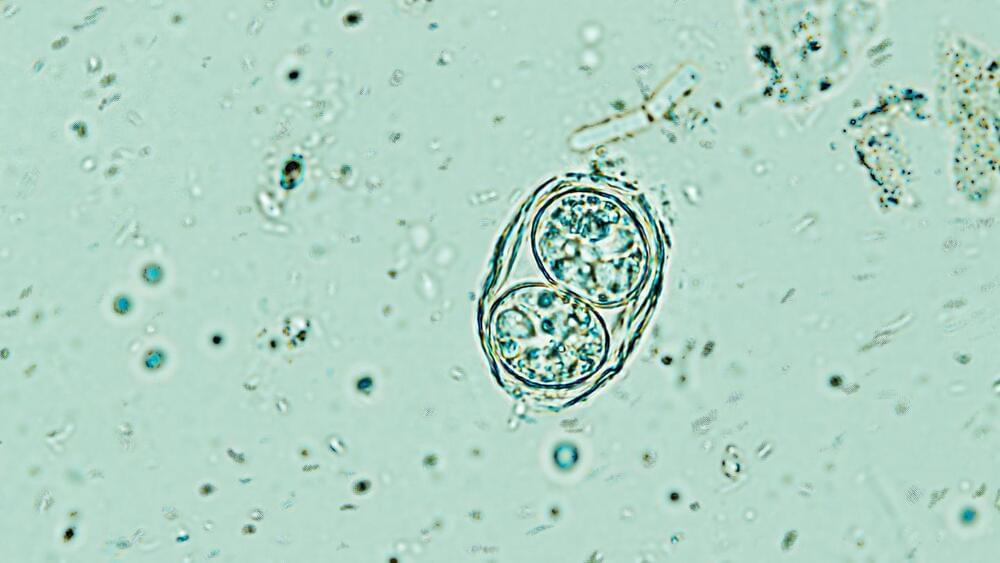
Electromagnetic wave pollution not only affects the normal operation of electronic equipment, greatly threatens the information security of the scientific community, but also endangers human health and is a possible cause of cancer and sensitized diseases.
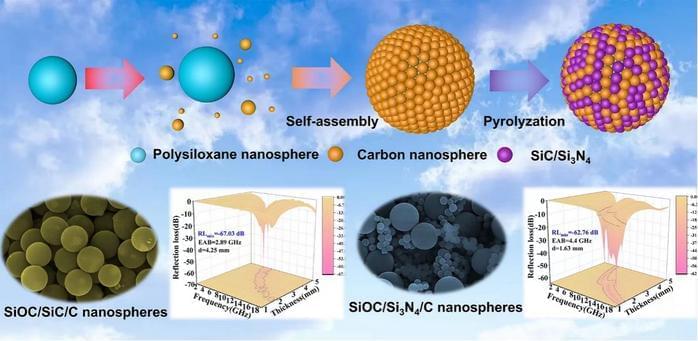
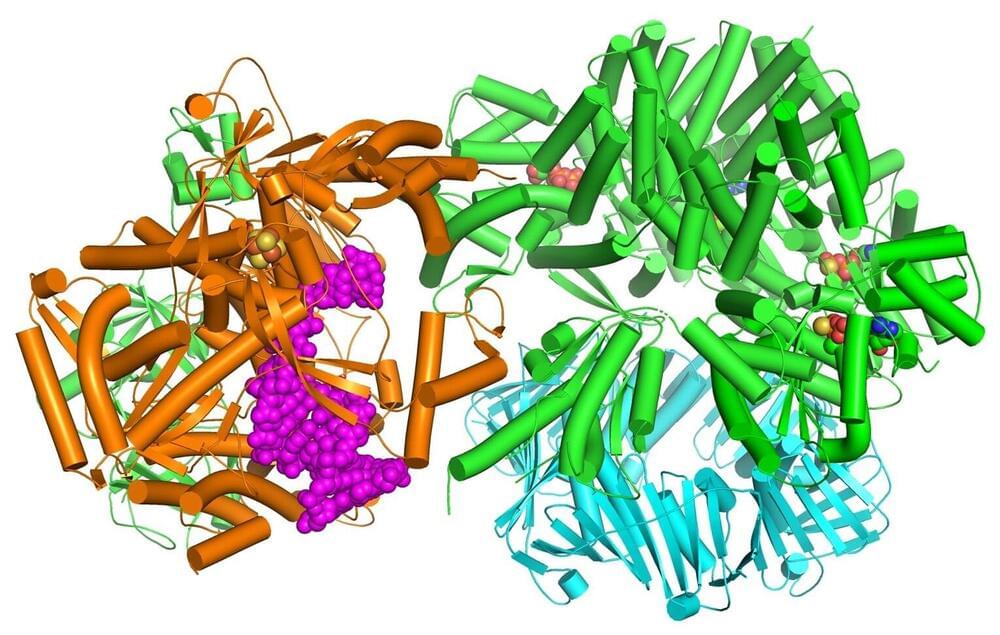
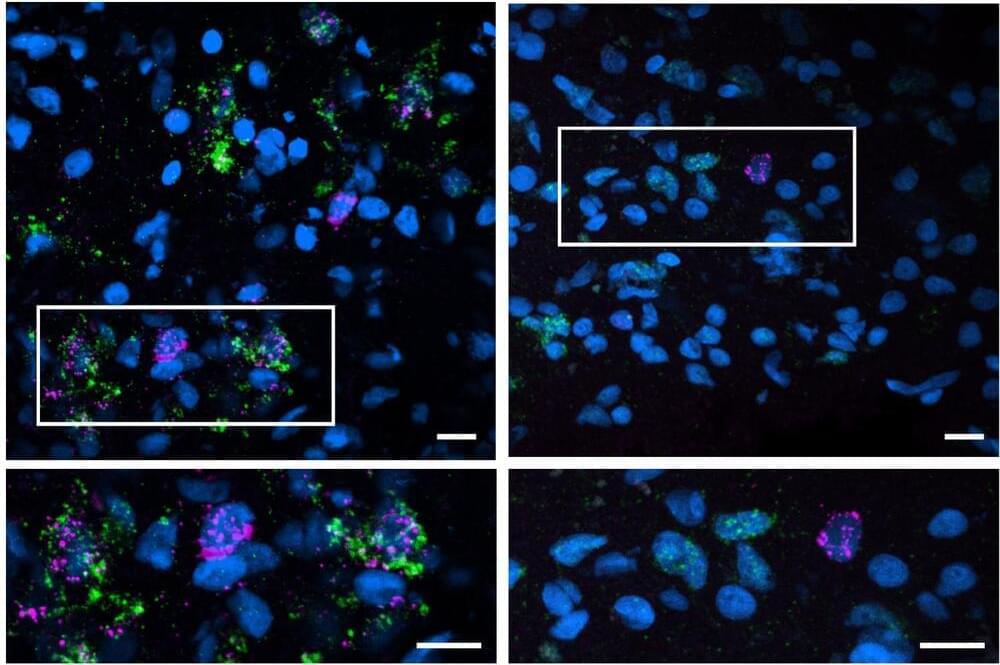
SiOC precursor ceramics have great application potential in electromagnetic protection because of their advantages such as lightweight, high-temperature resistance, and molecular designability. The main challenge of polymer-derived ceramic-based composites for electromagnetic wave absorption is the single loss mechanism, resulting in inferior electromagnetic wave attenuation ability.