Category: biotech/medical – Page 2,590
Cancer-like metabolism makes brain grow
The size of the human brain increased profoundly during evolution. A certain gene that is only found in humans triggers brain stem cells to form a larger pool of stem cells. As a consequence, more neurons can arise, which paves the way to a bigger brain. This brain size gene is called ARHGAP11B and so far, how it works was completely unknown. Researchers at the Max Planck Institute of Molecular Cell Biology and Genetics in Dresden now uncovered its mode of action. They show that the ARHGAP11B protein is located in the powerhouse of the cell—the mitochondria—and induces a metabolic pathway in the brain stem cells that is characteristic of cancer cells.
The research group of Wieland Huttner, a founding director of the Max Planck Institute of Molecular Cell Biology and Genetics, has been investigating the molecular mechanisms underlying the expansion of the brain during mammalian evolution for many years. In 2015, the group reported a key role for a gene that is only present in humans and in our closest extinct relatives, the Neanderthals and Denisovans. This gene, named ARHGAP11B, causes the so-called basal brain stem cells to expand in number and to eventually increase the production of neurons, leading to a bigger and more folded brain in the end. How the gene functions within the basal brain stem cells has been unknown so far.
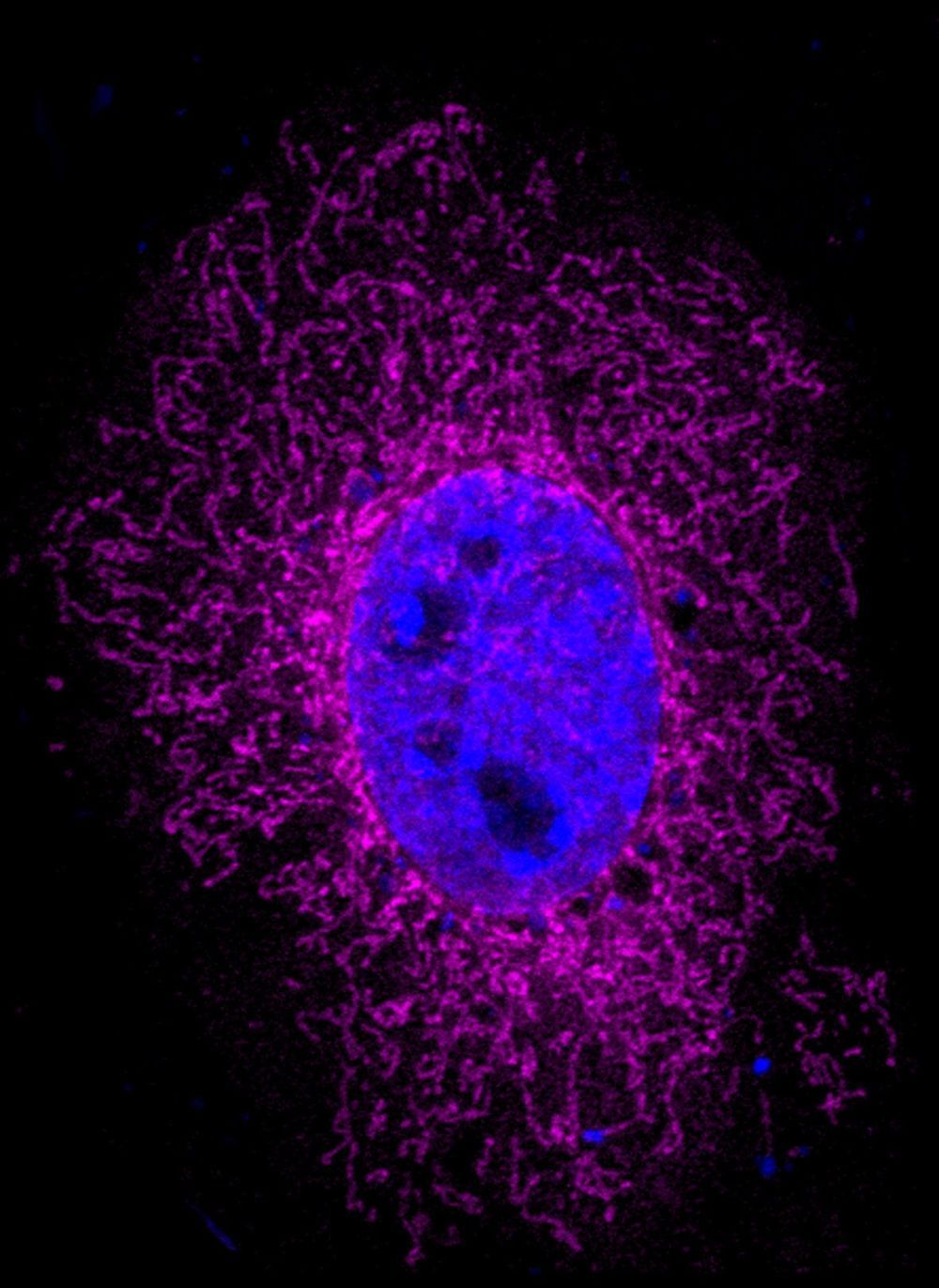
Takashi Namba, a postdoctoral scientist in the research group of Wieland Huttner, wanted to find the answer to this question, together with colleagues from the Max Planck Institute, the University Hospital Carl Gustav Carus Dresden, and the Department of Medical Biochemistry at the Semmelweis University, Budapest. He found that the ARHGAP11B protein is located in mitochondria, the organelles that generate most of the cell’s source of chemical energy and hence are often referred to as the powerhouse of the cell. Takashi Namba explains the results: We found that ARHGAP11B interacts with a protein in the membrane of mitochondria that regulates a membrane pore. As a consequence of this interaction, the pores in the membrane are closing up, preventing calcium leakage from the mitochondria. The resulting higher calcium concentration causes the mitochondria to generate chemical energy by a metabolic pathway called glutaminolysis.
The ‘Goldilocks’ principle for curing brain cancer
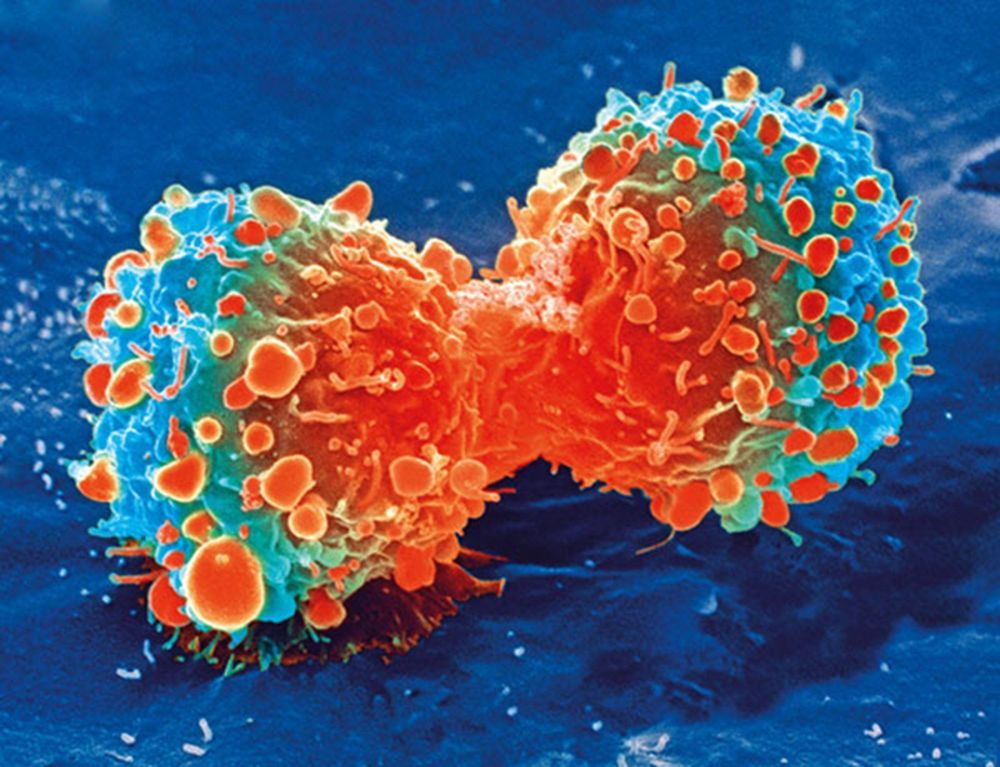
In the story of Goldilocks, a little girl tastes three different bowls of porridge to find which is not too hot, not too cold, but just the right temperature. In a study published in Advanced Therapeutics, University of Minnesota Medical School researchers report on a “Goldilocks” balance which holds the key to awakening the body’s immune response to fight off brain cancer.
The most common form of adult brain cancer is glioblastoma. Doctors diagnose about 14,000 glioblastoma cases in the U.S. each year. This aggressive cancer has claimed the lives of Senators John McCain and Edward Kennedy.
“Our body has armies of white blood cells that help us fight off bacteria, viruses and cancer cells. This constellation of cells constitute our immune system,” said senior author Clark C. Chen, MD, Ph.D., Lyle French Chair in Neurosurgery and Head of the Department of Neurosurgery at the University of Minnesota Medical School. “One of the key reasons why glioblastoma is so aggressive is that it shuts off this immune system.”

Treating Glaucoma with Senolytics
New research suggests that senolytic drugs, which remove harmful senescent cells that accumulate during aging, may be an effective therapy for glaucoma, a common age-related condition that leads to loss of vision.
In the short term, inflammation serves a useful purpose, as it helps to spur the repair and regeneration of tissue and rallies the immune system to defend against marauding invaders.
However, the chronic, smoldering, low-grade inflammation that occurs during aging can be incredibly harmful. The sources of this “inflammaging,” as some researchers describe it, include (but are not limited to) dysfunctional immune cells, cell debris, disruption to the gut microbiome, and senescent cells. Today, we are concerned about the latter after the release of a new study focusing on senescent cells and glaucoma [1].


How Alzheimer’s disease could be cured by shining light directly into the brain
Alzheimer’s disease could be reversed by shining light directly into the brain through the nose and skull, scientists believe.
The first major trial to see if light therapy could be beneficial for dementia has just begun following astonishing early results which have seen people regain their memory, reading and writing skills, and orientation.
If successful it would be the first treatment to actually reverse the disease. So far, even the most hopeful drugs, such as Biogen’s aducanumab, have only managed to slow the onset of dementia, and many scientists had given up hope of reversing brain damage once it had already happened.
Israeli treatment could delay deadly effects of ALS – new study
Specifically, AstroRx is a cell therapy product containing functional healthy astrocytes derived from human embryonic stem cells that aim to protect diseased motor neurons. The cells are injected in the patient through the spinal canal.
The company initiated its first ALS clinical trials in March 2018.
Prof. Michel Revel, founder and CEO of the company and winner of both the EMET Prize and the Israel Prize, said that the clinical trial results “provide the confidence needed to move forward” with cohorts B and C, which he said both “hold the potential for a prolonged response.”
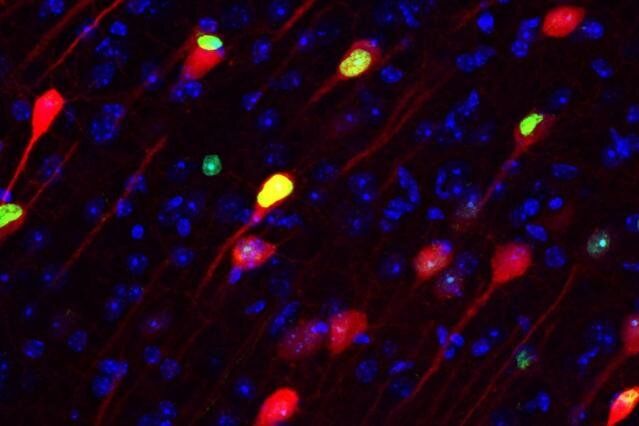
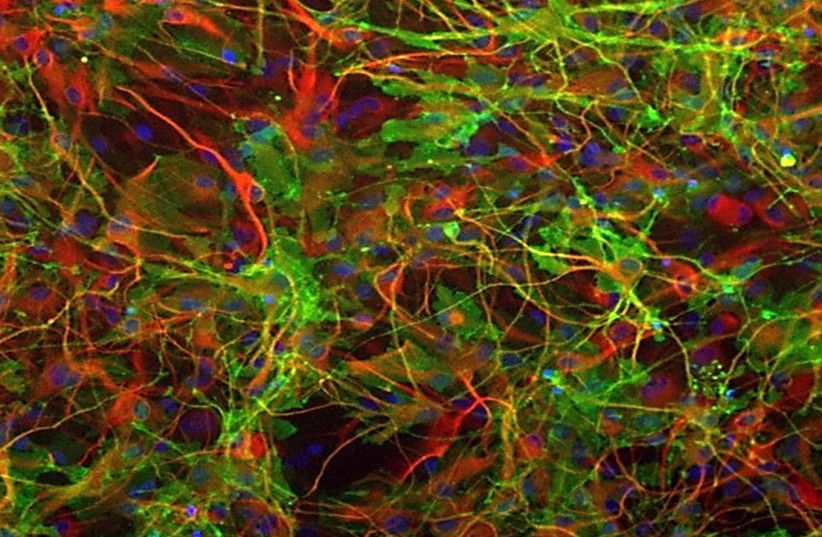
Engrams emerging as the basic unit of memory
Experiments in rodents have revealed that engrams exist as multiscale networks of neurons. An experience becomes stored as a potentially retrievable memory in the brain when excited neurons in a brain region such as the hippocampus or amygdala become recruited into a local ensemble. These ensembles combine with others in other regions, such as the cortex, into an “engram complex.” Crucial to this process of linking engram cells is the ability of neurons to forge new circuit connections, via processes known as “synaptic plasticity” and “dendritic spine formation.” Importantly, experiments show that the memory initially stored across an engram complex can be retrieved by its reactivation but may also persist “silently” even when memories cannot be naturally recalled, for instance in mouse models used to study memory disorders such as early stage Alzheimer’s disease.
“More than 100 years ago Semon put forth a law of engraphy,” wrote Josselyn, Senior Scientist at SickKids, Professor of Psychology and Physiology at the University of Toronto and Senior Fellow in the Brain, Mind & Consciousness Program at the Canadian Institute for Advanced Research, (CIFAR) and Tonegawa, Picower Professor of Biology and Neuroscience at the RIKEN-MIT Laboratory for Neural Circuit Genetics at MIT and Investigator of the Howard Hughes Medical Institute. “Combining these theoretical ideas with the new tools that allow researchers to image and manipulate engrams at the level of cell ensembles facilitated many important insights into memory function.”
“For instance, evidence indicates that both increased intrinsic excitability and synaptic plasticity work hand in hand to form engrams and that these processes may also be important in memory linking, memory retrieval, and memory consolidation.”
For as much as the field has learned, Josselyn and Tonegawa wrote, there are still important unanswered questions and untapped potential applications: How do engrams change over time? How can engrams and memories be studied more directly in humans? And can applying knowledge about biological engrams inspire advances in artificial intelligence, which in turn could feedback new insights into the workings of engrams?
A review in Science traces neuroscientists’ progress in studying the neural substrate for storing memories and raises key future questions for the field.