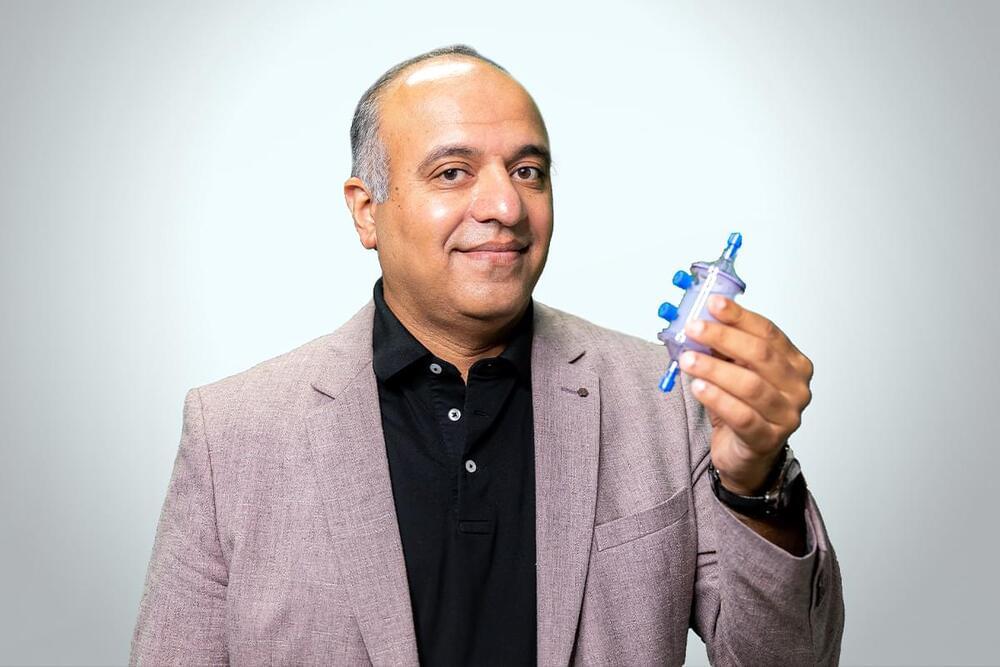
San Diego based biotech Immunicom has developed an innovative therapeutic device that is intended to remove specific factors from blood that prevent our immune systems from fighting disease. Existing “therapeutic apheresis” treatments usually involve modification to cells harvested from patients or some form of plasma exchange. Immunicom’s technology uses a similar treatment procedure but says its approach of “capturing” targeted molecules is very different from other treatments.
Immunicom creates customised molecules that are designed to capture specific proteins or cytokines, but instead of turning those into drugs, it deploys them via its proprietary cartridges, which are essentially small liquid filters that can be fitted into any plasmapheresis machine. In a treatment similar to dialysis, the cartridges are used to treat a patient’s blood and plasma outside their body, reducing the levels of the target factors, with the goal of enabling the immune system to fight disease.
While Immunicom has focused its initial efforts on treatments for cancer, the company claims its technology can also potentially be applied to longevity and the treatment of a wide range of age-related diseases.