DNA sequencing technology, i.e., determining the order of nucleotide bases in a DNA molecule, is central to personalized medicine and disease diagnostics, yet even the fastest technologies require hours, or days, to read a complete sequence. Now, a multi-institutional research team led by The Institute of Scientific and Industrial Research (SANKEN) at Osaka University, has developed a technique that could lead to a new paradigm for genomic analysis.
DNA sequences are sequential arrangements of the nucleotide bases, i.e., the four letters that encode information invaluable to the proper functioning of an organism. For example, changing the identity of just one nucleotide out of the several billion nucleotide pairs in the human genome can lead to a serious medical condition. The ability to read DNA sequences quickly and reliably is thus essential to some urgent point-of-care decisions, such as how to proceed with a particular chemotherapy treatment.
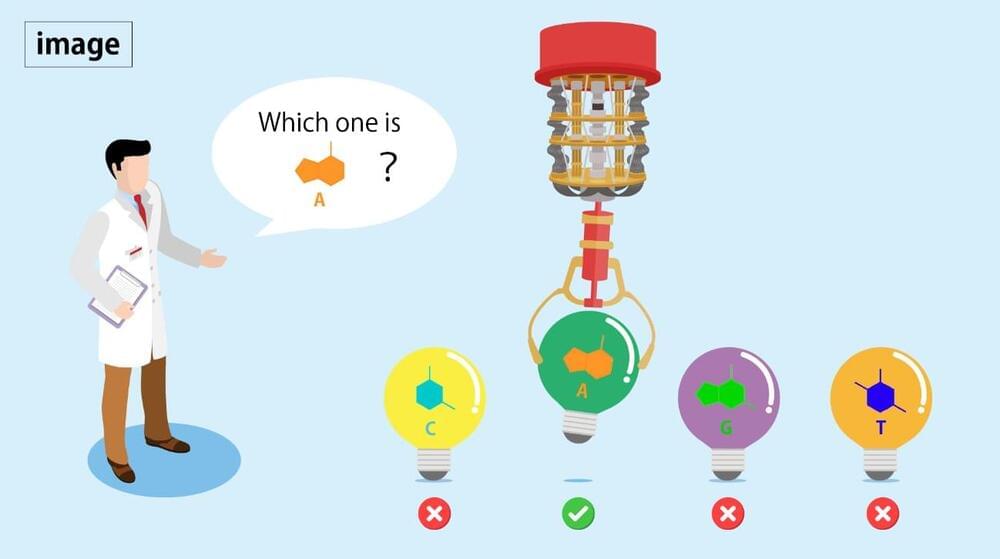
Unfortunately, genome analysis remains challenging for classical computers, and it’s in this context that quantum computers show promise. Quantum computers use quantum bits instead of the zeroes and ones of classical computers, facilitating an exponential increase in computational speed.