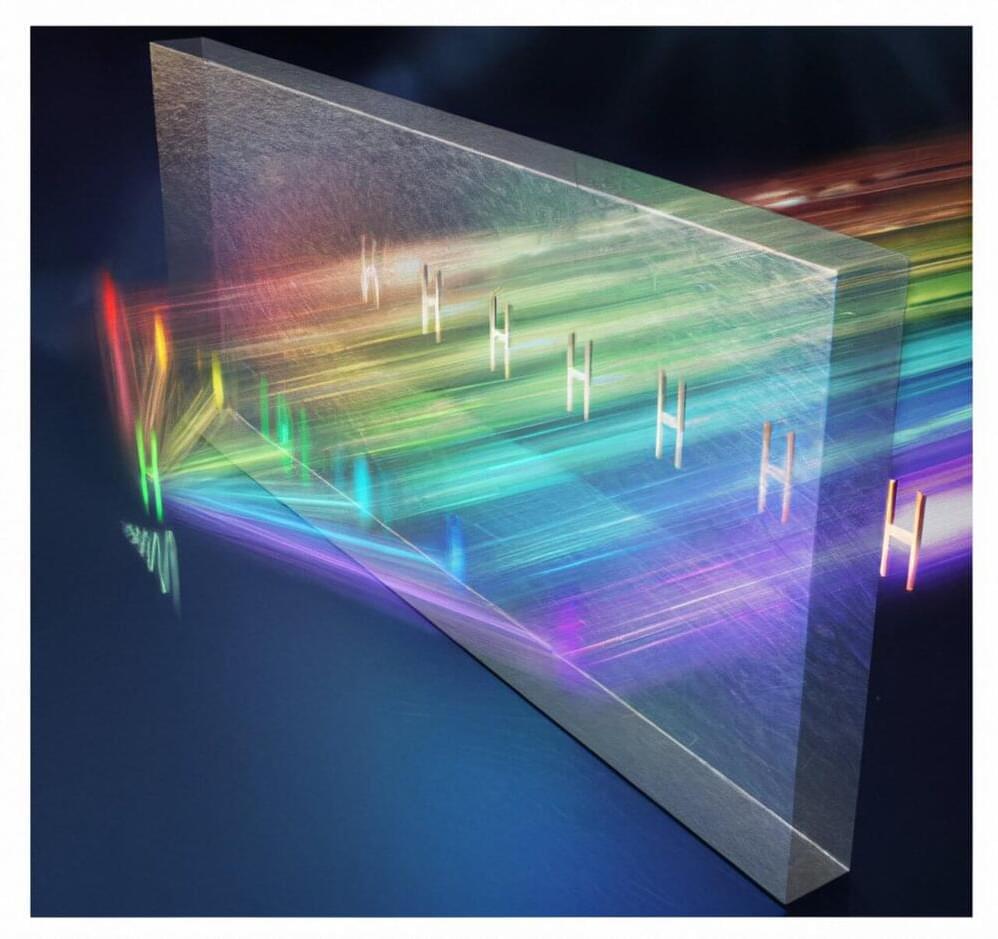
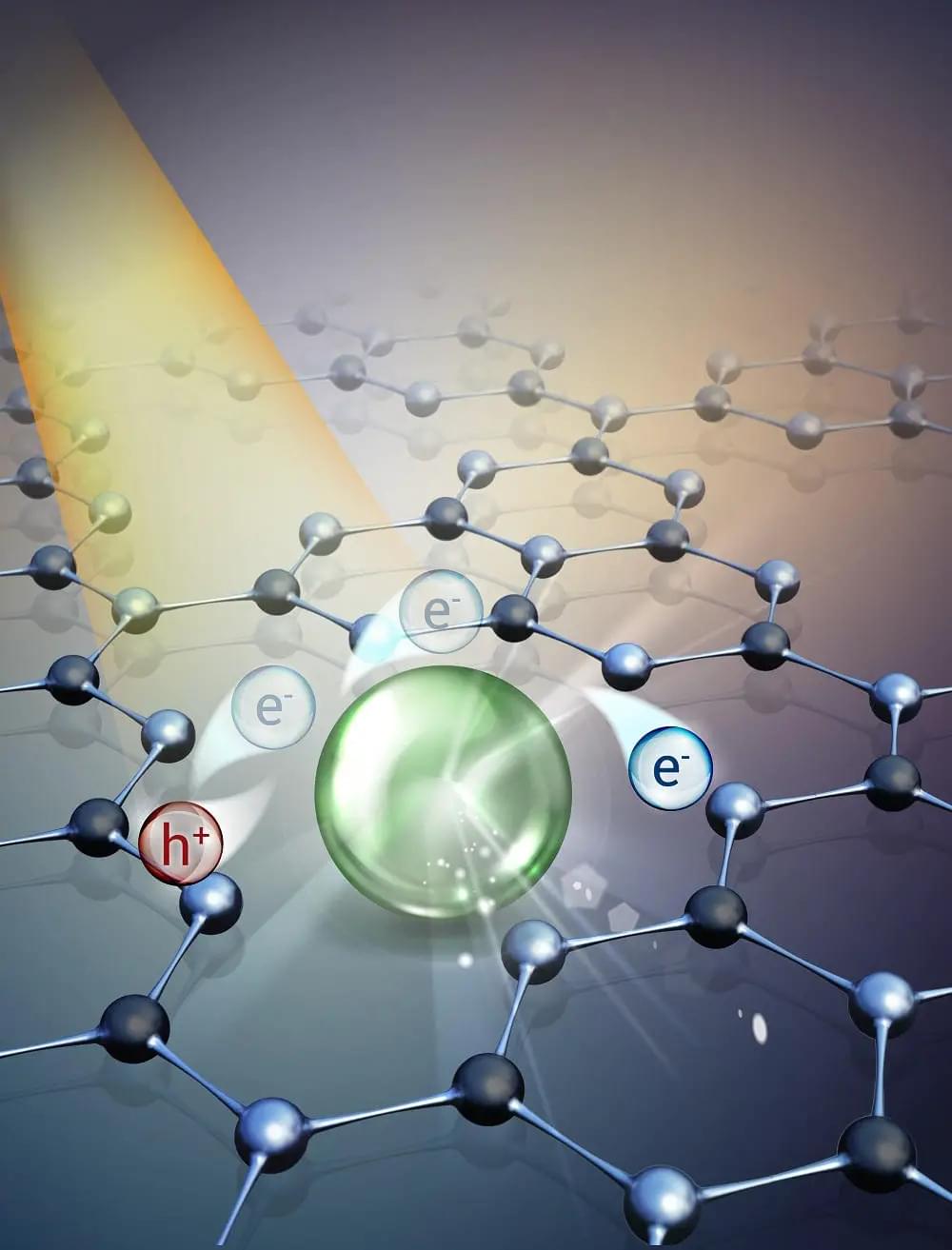
A collaborative research team led by Interim Head of Physics Professor Shuang Zhang from The University of Hong Kong (HKU), along with National Center for Nanoscience and Technology, Imperial College London and University of California, Berkeley, has proposed a new synthetic complex frequency wave (CFW) approach to address optical loss in superimaging demonstration. The research findings were recently published in the journal Science.
Imaging plays an important role in many fields, including biology, medicine and material science. Optical microscopes use light to obtain imaging of miniscule objects. However, conventional microscopes can only resolve feature sizes in the order of the optical wavelength at best, known as the diffraction limit.
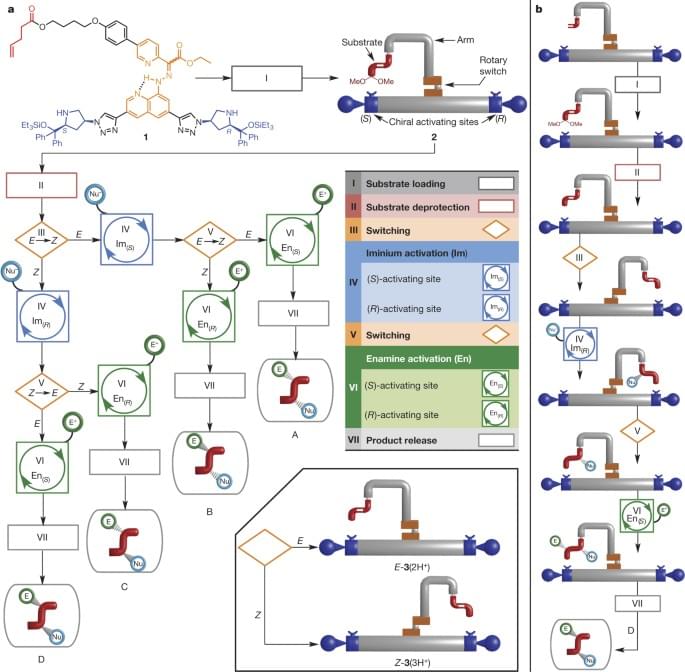
To overcome the diffraction limit, Sir John Pendry from Imperial College London introduced the concept of superlenses, which can be constructed from negative index media or noble metals like silver. Subsequently, Professor Xiang Zhang, the current President and Vice-Chancellor of HKU, along with his then team at the University of California, Berkeley, experimentally demonstrated superimaging using both a silver thin film and a silver/dielectric multilayer stack.