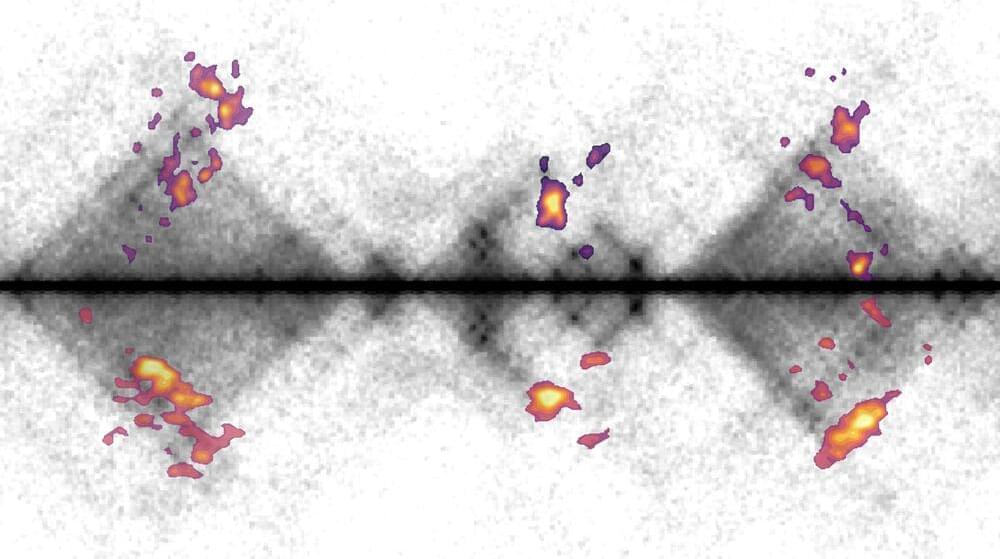
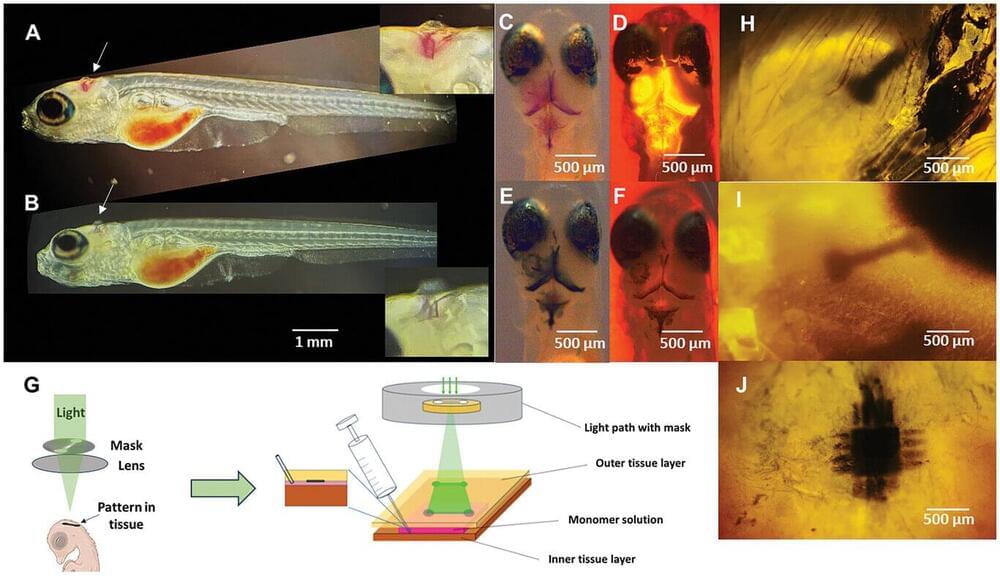
Summary: Researchers have demonstrated how brain activity can predict behavior in urban environments, providing a roadmap for improving urban planning. Using functional MRI scans, the study identified activity in the brain’s reward system, specifically the ventromedial prefrontal cortex, as a key predictor of why people visit certain urban areas.
Participants rated photos of Lisbon’s urban spaces, and their brain responses were linked to visitation patterns, showing that people are drawn to areas of perceived value. This research suggests urban design can prioritize environments that align with cognitive and emotional well-being.
Neurourbanism, the emerging field behind this study, offers tools to design cities that enhance livability and sustainability. By focusing on human-centered approaches, cities can improve efficiency, mobility, and resident happiness.