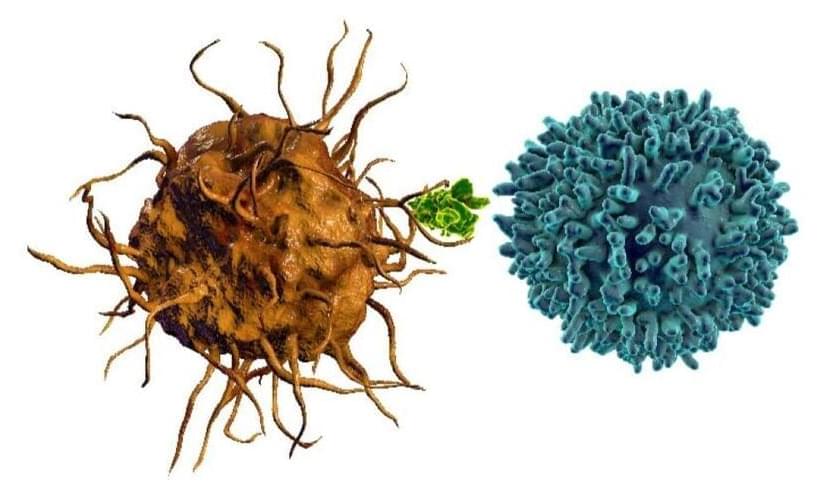
Chimeric antigen receptor (CAR) therapies involve the use of engineered receptors capable of redirecting immune cells to recognize and destroy cancer cells expressing a specific antigen. Currently, CAR-T cells, T cells equipped with CAR, dominate the field of CAR therapy. Since 2017, over 700 clinical trials involving CAR-T therapy have been registered and the U.S. Food and Drug Administration (FDA) has approved six CAR-T therapies for the treatment of leukemia, lymphomas, and multiple myeloma (Fig. 1) [1]. However, despite its clinical significance, several factors contribute to the limitations of CAR-T therapy. First, as collecting T cells is costly and time-consuming, this may not be feasible for patients already suffering from a compromised immune system. Second, CAR-T therapies mainly focus on treating hematological malignancies, having limited effectiveness in treating solid tumors. Third, CAR-T cells struggle to penetrate the tumor microenvironment (TME), which can hinder their therapeutic function. To overcome these limitations, promising CAR designs have emerged for multi-target CAR-T alongside novel therapies that utilize other immune cell types such as CAR-Natural killer (NK) and CAR-Macrophage (M) cells.
Figure 1. Timeline of CAR-T FDA approvals in the US. B-ALL, B cell acute lymphoblastic leukemia; LBCL, large B cell lymphoma; MCL, mantle cell lymphoma; MM, multiple myeloma; R/R, relapsed/refractorySource: adapted from Maakaron, J, et al. 2022[1].